

The process of obtaining dental implants is intricate and involves several critical stages that ensure a successful outcome. It commences with an initial consultation, during which a thorough evaluation of both oral health and medical history is performed.
This assessment lays the groundwork for a tailored treatment plan, addressing individual needs and anatomical considerations.
As one progresses through the various phases, including pre-surgery preparation and the implant placement itself, understanding each step becomes vital. What happens during recovery, and how does it influence the final restoration?
The initial consultation is a crucial step in the journey toward obtaining dental implants, as it lays the foundation for successful treatment. During this appointment, the dental professional conducts a comprehensive assessment of the patient's oral health, including a review of medical history, examination of the gums and remaining teeth, and evaluation of bone density.
Diagnostic imaging, such as X-rays or 3D scans, may also be performed to visualize the jaw structure and identify any potential complications. This thorough evaluation allows the dentist to determine the patient's suitability for implants and discuss any necessary preparatory procedures.
Additionally, the initial consultation serves as an opportunity for patients to ask questions, express concerns, and gain a clear understanding of the dental implant process.
After the initial consultation, the next phase involves meticulous treatment planning, which is pivotal to the success of dental implant procedures. During this stage, the dental team conducts a comprehensive evaluation, including diagnostic imaging such as X-rays or 3D scans, to assess the jawbone's condition and the spatial relationship of surrounding teeth.
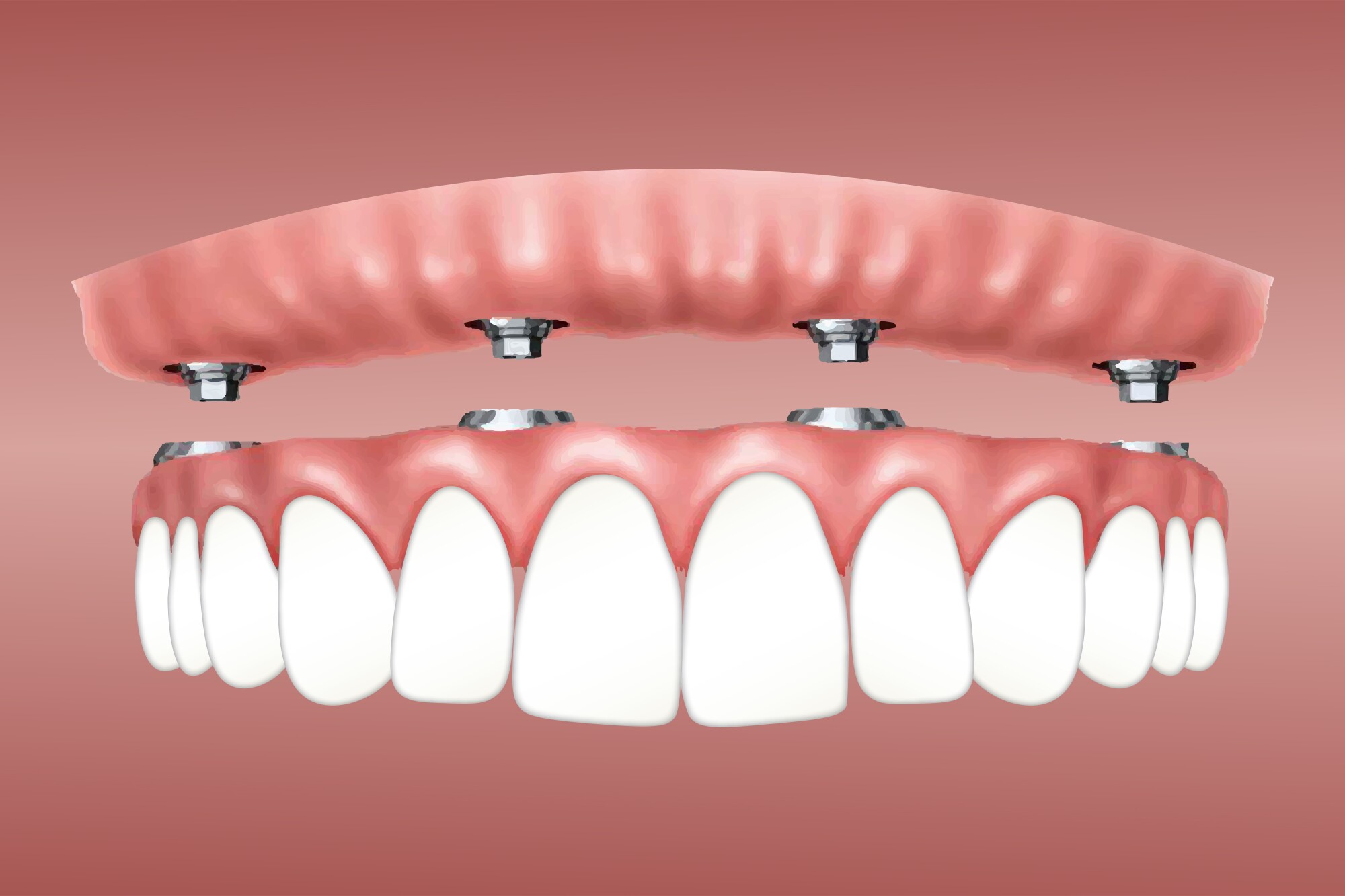
This information is crucial for determining the appropriate type and placement of the implants. A customized treatment plan is then developed, outlining the number of implants required, the timeline for the procedure, and any additional treatments needed, such as bone grafting.
Effective communication between the patient and dental professionals is essential, ensuring that expectations are managed and the plan aligns with the patient's oral health goals and lifestyle.
Preparation for dental implant surgery is a critical step that significantly influences the procedure's success. Prior to the surgery, patients should undergo a thorough medical evaluation, including dental X-rays and possibly a CT scan, to assess jawbone health and determine the optimal implant placement.
Patients are advised to disclose their complete medical history, including medications and allergies, to ensure a safe surgical environment. Additionally, it is essential to avoid blood-thinning medications, smoking, and alcohol consumption in the days leading up to the procedure.
Following the dentist's pre-operative guidelines, such as dietary restrictions and medication management, will help minimize complications and enhance recovery. Lastly, arranging for post-surgery transportation is crucial, as the procedure may involve sedation.
During the implant placement procedure, the dentist begins by administering local anesthesia to ensure the patient remains comfortable and pain-free throughout the process.
The next step involves making a small incision in the gum tissue to expose the jawbone. Once the bone is accessible, the dentist drills a precise hole where the dental implant will be placed.
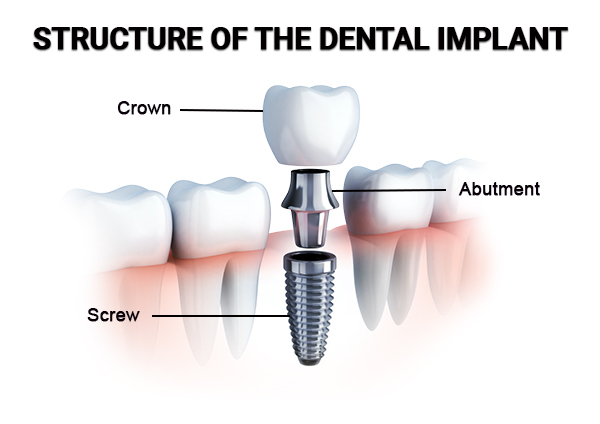
The titanium implant, designed to integrate with the bone, is then carefully inserted into this hole. After the implant is positioned correctly, the gum tissue is stitched back into place, covering the implant. This initial placement is critical for the subsequent healing phase, during which the bone will grow around the implant, providing stability and support for the future crown.
Recovering from dental implant surgery is a crucial phase that significantly impacts the success of the procedure. Post-operative care involves managing discomfort, swelling, and maintaining oral hygiene.
Patients are typically advised to rest for the first 24 hours, applying ice packs to reduce swelling. Over-the-counter pain relievers can help alleviate discomfort, while prescribed medications should be taken as directed.
It is essential to follow a soft food diet for several days, avoiding hard or chewy items that may disrupt healing. Patients should maintain oral hygiene by gently brushing their teeth and rinsing with a prescribed mouthwash. Regular follow-up appointments with the dentist are vital to monitor healing and ensure the implant is integrating properly with the jawbone.
Once healing from the initial dental implant surgery is complete, the final restoration process can commence. This stage typically involves the attachment of a custom-made crown to the abutment, which connects the implant to the crown. Your dentist will take precise impressions of your mouth to create a crown that matches the shape, size, and color of your natural teeth, ensuring optimal aesthetics and function.
After the crown is fabricated, it is securely placed onto the abutment, and adjustments may be made for a perfect fit. Patients will receive instructions for care and maintenance to ensure the longevity of the restoration.
A successful final restoration restores full function and enhances the appearance of the smile, providing confidence and comfort in daily activities.

If a dental implant fails, it can result in pain, infection, or loss of the implant itself. Common causes of failure include insufficient bone density, improper placement, or infection. When an implant fails, a thorough evaluation is necessary to determine the underlying cause. In many cases, the implant can be removed, and after addressing the issues, patients may be eligible for a new implant or alternative tooth replacement options.
The cost of dental implants can vary significantly based on several factors, including geographical location, the complexity of the case, and the materials used. On average, the cost for a single dental implant ranges from $3,000 to $4,500, which typically includes the implant, abutment, and crown. Additional expenses may arise from preliminary procedures, such as bone grafting or sinus lifts, which can increase the overall investment in achieving optimal dental restoration.
Dental implants are not universally suitable for everyone. Factors such as age, overall health, bone density, and specific dental conditions significantly influence candidacy. Individuals with uncontrolled diabetes, certain autoimmune disorders, or those who smoke excessively may face complications. A thorough evaluation by a dental professional is essential to determine if implants are appropriate. Ultimately, personalized assessments ensure optimal outcomes and patient safety in the pursuit of restorative dental solutions.